By Kathy Ruscitto, Advisor
Friday, June 17, 2022

We have made many advancements in health care these days. Whether this involves staffing, healthcare delivery and access, or new technology and a growing sophistication with vaccines, all of these milestones benefit the patient.
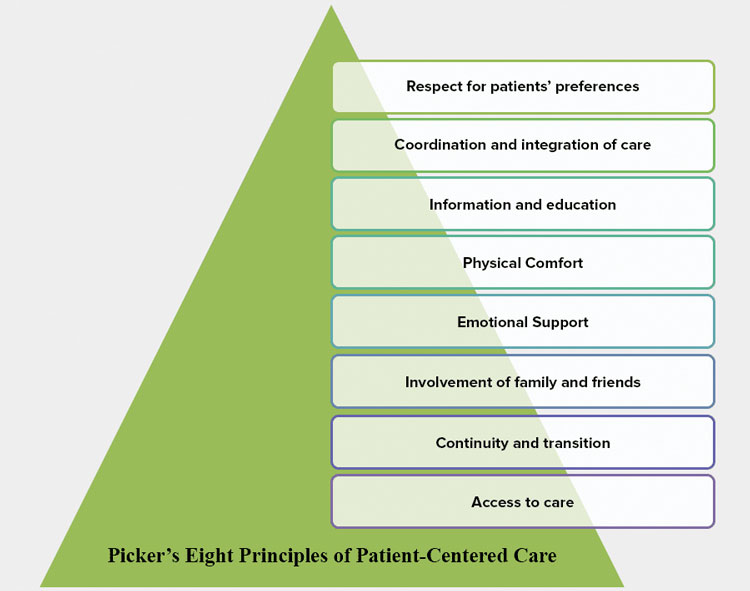
Patient-centered care has emerged as the preferred healthcare framework for providing services that are effective and produce the best outcomes. Patient-centered care is more than listening and engaging the patient in their care. It also involves developing processes and making administrative decisions that improve the overall patient experience — from how a reception area is designed and how patient data is analyzed to education and communication about a diagnosis and even how a bill is explained. Most importantly, patient- or people-centered care means how the elements of the care team and social determinants are connected across time, place and discipline. That collaboration is what is so important to patients.
Connecting the Dots
We have developed a high level of specialized clinical expertise, but often the parts don’t connect. A patient with MS sees a neurologist for falls, an orthopedic surgeon for joint pain and a primary care physician for general concerns. Without some way to integrate all of this care, the patient is often left navigating a system they don’t entirely understand.

Kathy Ruscitto, Advisor
Health care must be evidence-based and patient-centered, which can be a complicated balancing act. But if the clinician understands the standards of care and how to effectively communicate them, the patient feels listened to and can better address all of their needs with the provider.
The World Health Organization has commenced a worldwide initiative to introduce patient-centered approaches in every country, meaning patient-centered care is now internationally accepted as a best practice framework.
However, to every clinician, every practice and every organization, the words patient-centered care may take on a different meaning. For example, clinical approaches to diagnosing and treating Lyme disease differ between the Infectious Disease Society of America and the International Lyme and Associated Diseases Society. The patient-centered approach calls for any clinician to listen to where the patient is with symptoms and offer care that considers all approaches.
The Institute of Medicine defines patient-centered care as: “Providing care that is respectful of and responsive to individual patient preferences, needs and values, and ensuring that patient values guide all clinical decisions.” It starts with listening deeply to the challenges and needs of every patient, particularly of those with chronic conditions.
Patient-centered care helps set up a collaborative dynamic that meets patients’ needs. When done well, it’s a win for clinicians, a win for patients and a win for payers because this care model improves health outcomes.
Finally, and probably worthy of another discussion itself, how can we use technology to create virtual care teams around chronic conditions and improve our care plans?
Resources
- Institute for Patient and Family Centered Care (ipfcc.org/)
- Patient Engagement HIT (patientengagementhit.com/news/what-does-patient-centered-care-truly-mean)
Kathryn Ruscitto, Advisor can be reached at linkedin.com/in/kathrynruscitto or at krusct@gmail.com.